Mpox is an infection caused by the Monkeypox virus, which is in the same virus family as the one that causes smallpox. Individuals infected with M-pox often develop a painful rash, along with a variety of additional symptoms. This rash goes through various stages before developing scabs and healing fully. The rashes may be confused with other viral infections such as chicken pox, measles, handfoot mouth disease, and so on.
On August 14, 2024, the World Health Organization designated the epidemic in portions of Africa a public health emergency of worldwide concern. The Democratic Republic of the Congo (DRC) is now experiencing a severe outbreak. Children are at a larger risk of contracting than adults. According to the World Health Organization (WHO), 70% of the 14,901 cases in the Democratic Republic of the Congo (DRC) involved children under the age of 15, with 39% affecting children under five. Children in the Democratic Republic of the Congo have approximately four times the death rate as adults. The most current variety of M-pox, clade 1b, was discovered in the Democratic Republic of the Congo in September 2023 and has since spread to neighboring nations.
How to Recognise Mpox?
Dr. Manu Chaudhary, Consultant, Pediatric Infectious Diseases Specialist, Rainbow Children’s Hospital, Marathahalli, Bangalore, describes the typical symptoms of Mpox as a rash with painful pus-filled lesions on the face, hands, and soles. Other typical symptoms include fever, swollen lymph nodes, a sore throat, headache, muscle aches, back pain, and low energy. Identifying these symptoms will help you obtain the assistance you require straight away.
How does M-pox spread?
- M-pox is closely related to the smallpox virus, eradicated globally in 1980.
- The virus can spread through close contact with an infected animal or person.
- Human-to-human transmission often occurs through skin-to-skin contact with someone who has a rash, sores, or scabs.
- The virus can also spread via respiratory droplets or oral fluids during intimate sexual activities, including kissing, and oral, anal, or vaginal sex.
- Infection can be transmitted through contact with contaminated fabrics, objects, or surfaces, such as clothing, bedding, or towels.
- A patient of Mpox can spread infection till all scabs fall off and a new layer of skin forms (~3 weeks)
- Time from exposure to developing symptoms can vary from 5-21 days
Treatment For Mpox
Mpox patients should seek medical attention if they have traveled to Central or West African countries, have come into touch with someone who has been proven or suspected of having the disease, or are men who have close or personal contact with other men. It is critical to notify the hospital ahead of time so that isolation may be set up and the virus does not spread to healthcare personnel or other patients.
There are currently no specific therapies for this, therefore people who have been diagnosed with the virus should isolate themselves at home and avoid intimate contact until their skin sores heal. Severe instances, immunocompromised people, pregnant, breastfeeding, or children under the age of eight may require antiviral or antibody therapy, such as intravenous vaccinia immune globulin. Tecovirimat (TPOXX) is an antiviral treatment for severe cases, while cidofovir and IVIG are other options for children and immunocompromised patients.
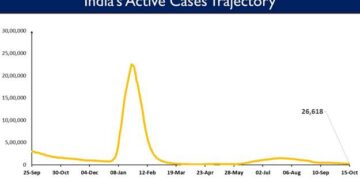
According to the Ministry of Health and Family Welfare, 30 cases of mpox have been reported in India since 2022, the most recent occurring in March 2024. Although vaccines like JYNNEOS and LC16 provide some protection against mpox, they are not widely distributed in India. This event highlights the importance of keeping vigilant public health measures and raising awareness while avoiding excessive panic.
Source:In






 Finance
Finance







